A. Unless delivery is imminent, transport to a hospital with obstetrical capabilities.
B. Imminent delivery i
s when the baby’s head is visible at the vaginal opening during a
contraction (crowning).
C. A visual inspection of the perineal area should onl
y be done when contractions are less than
5 minutes apart, there is bleeding / fluid discharge and/or the patient feels the urge to push.
Do not perform a digital examination to gauge cervical dilation.
D. The E
MT should only place a gloved hand inside of the vagina as indicated for breech
del
ivery with an entrapped head or prolapsed umbilical cord.
E. A m
other in active labor should be placed on the cot or floor to prevent the newborn from
falling after delivery.
A. Obtain hi
story of patient condition and pregnancy: contraction duration and interval, due date,
total number of pregnancies (G - Gravida), and number of deliveries of live child (P – Parity)
,
num
ber of abortions or miscarriages (A), prenatal care, and any complications during this
pregnancy or previous pregnancies (e.g. HTN, eclampsia).
B. Determine i
f you’re going to transport or stay on-scene for delivery. Transport unless
crowning is present during a contraction. Contact Medical Control.
C. Always t
ry to transport the mother to her designated hospital for delivery. Transport mother
on left side with head slightly elevated to relieve pressure on the mother’s vena cava.
D. If delivery is
imminent, prepare equipment and follow delivery guidelines.
E. Normal P
resentation Childbirth Delivery Guidelines:
1. Gather equi
pment – OB kit, oxygen, BVM, towels, blankets, large dressings, cot and
PPE.
2. Place patient on c
ot or floor on her back with knees and hips flexed.
3. If t
ime permits, drape mother with towels in OB kit.
4. Don sterile gloves, gown and face s
hield.
5. As head crowns, gentle pr
essure with a flat hand on the baby’s head should be
applied to prevent an explosive delivery.
6. Support head as it del
ivers.
7. Slide fingers along neck to check f
or the umbilical cord.
a. If present, try t
o slip the cord over baby’s head.
b. If unable and cord is wrapped too t
ightly for delivery to proceed, clamp cord
in 2 places and cut between.
8. Put hands
on either side of infant’s head with thumbs towards the face.
9. Gently guide head downward to assist with del
ivery of anterior (top) shoulder. Do
NOT pull! Doing so can cause damage to spinal nerves.
a. If shoulder does not deliver, see D
elivery Complications Guidelines –
Shoulder Dystocia.
Effective 1/10/23
Replaces 7/1/19
Childbirth and OB Emergencies Page 1 of 7
CHILDBIRTH and OBSTETRICAL
EMERGENCIES
GENERAL CONSIDERATIONS FOR CHILDBIRTH
Basic EMT
Effective 1/10/23
Replaces 7/1/19
Childbirth and OB Emergencies Page 2 of 7
10. Gently guide head upward to allow delivery of posterior (bottom) shoulder.
11. After the shoulders are delivered the rest of the body usually follows quickly, s
o be
s
ure to support the body as it emerges. Infant will be slippery. Do NOT put fingers i
n
ar
mpits to pull the body out. Record time of baby’s birth.
12. Suction baby’s mouth then nose if necessary to clear airway before stimulating the
baby to breathe. See NRP below.
13. Keep baby at level of vagina to prevent over- or under-transfusion of blood from the
cord.
14. Clamp cord in two places about 6-8 inches from the abdomen and cut between
clamps with scissors. Do not milk the cord. You do not have to wait for the cord to
stop pulsating.
15. Immediately start drying the baby with towels.
16. Assess mother and baby for complications.
17. Obtain APGAR scores at one and five minutes after delivery.
18. The placenta may deliver any time in the next 20-30 minutes. You do not have to wait
on-scene for placental delivery to transport the mother. Apply a VERY GENTLE,
continuous pull on the placental cord and it will eventually deliver. DO NOT RUSH, DO
NOT PULL HARD on the cord as this can cause the uterus to invert or cause t
he
pl
acenta to separate from the uterus, either of which can cause hemorrhage. If
placenta does deliver, transport in biohazard bag with patient.
19. Baby should be dried, placed skin-to-skin with the mother, and covered with dry li
nen
t
o maintain temperature.
20. Observation of breathing, activity, and color should be ongoing.
21. Keep mother and baby warm.
22. Transport
A. Start IV of normal saline if hypovolemic shock or excessive bleeding is present. A
dminister
500-1000 mL bolus and repeat as needed.
B. Paramedics should administer T
XA for patients ≥ 12 yo for post-partum bleeding
unresponsive to uterine massage and IV fluid resuscitation
A. Contact Medical Control as soon as any complication is di
scovered.
B. Breech Delivery – F
ootling Breech (one or both feet delivered first) and Frank Breech
(buttocks are presenting part)
1. When feet or buttocks are first noted at the vaginal opening during a contraction,
there is normally time to transport patient to nearest facility.
2. If upper thighs or buttocks have passed out of vagina, delivery is imminent and baby
should be delivered on-scene/in the house.
3. Breech Infant Delivery Guidelines:
a. Gather equipment – OB kit, oxygen, BVM, towels, blankets, large dressings,
cot and PPE.
b. Place patient on cot or floor on her back with knees and hips flexed.
c. If time permits, drape mother with towels in OB kit.
d. Don sterile gloves, gown and face shield.
e. Allow baby to deliver with contractions while supporting the body. T
he
pos
terior or bottom buttock and hip usually deliver first, then the anterior hip.
Advanced EMT / Paramedic
DELIVERY COMPLICATIONS
Effective 1/10/23
Replaces 7/1/19
Childbirth and OB Emergencies Page 3 of 7
f. After leg delivery, hold onto pelvis with both hands to support the body which
will naturally turn to deliver the shoulders.
g. If the shoulders do not deliver easily, apply gentle traction of the body until
the axilla become visible. Then guide the infant’s body upward to deliver the
posterior (bottom) shoulder. Guide the infant downward to deliver the
anterior (top) shoulder.
h. As the head passes the pubis, usually face down, put one hand on the face
and the other on the back of the neck, apply gentle upward traction until the
mouth appears.
i. If the baby’s body has delivered and the head appears to be caught in vagina,
the EMT must support the baby’s body and insert two fingers into the vaginal
opening along the baby’s neck until the chin is located. At this point, the two
fingers should be placed between the chin and the vaginal wall and advanced
past the mouth and nose.
j. After achieving this position, a passage for air must be created by pushing
the vaginal wall away from the baby’s face. The air passage must be
maintained until the baby is completely delivered, no matter how long that
takes.
k. After delivery follow routine neonatal assessment.
C. Shoulder Dystocia – after delivery of the head, top/anterior shoulder gets stuck and delivery
is halted.
1. If unable to deliver anterior shoulder, have mother flex hips and bring knees to her
chest to change the angle of the pelvis (McRoberts Maneuver)
2. Have an assistant put moderate pressure on abdomen just above the symphis pubis.
3. If this does not assist in delivery of shoulder, the transport immediately.
CI. Excessive Bleeding Pre-Delivery
1. Follow Hypovolemic Shock Protocol in addition to normal delivery guidelines.
2. If delivery is not imminent, patient should be transported on her left side and follow
Hypovolemic Shock Protocol
CII. Excessive Bleeding Post-Delivery
1. Start IV normal saline. Administer 500-1000 mL bolus and repeat as needed.
2. Typically caused by uterine atony. If placenta has been delivered, massage uterus
and put baby to mother’s breast.
3. If the uterus has inverted and is extending through the cervix it must be replaced
quickly to limit profound hemorrhage. With the palm of the hand, push the fundus of
the inverted uterus toward the vagina. If this does not turn the uterus right-side out,
cover the uterus with moistened towels and transport immediately.
4. Paramedics should administer TXA for patients ≥ 12 yo for post-partum bleeding
unresponsive to uterine massage and IV fluid resuscitation
CIII. Prolapsed Cord – the umbilical cord has passed through the vagina and is exposed.
1. Patient should be transported with hips elevated or in knee-to-chest position. Place
moist dressing around the cord.
2. If umbilical cord is seen or felt in the vagina, insert two fingers to elevate presenting
part away from the cord to stop baby from crushing its own blood/oxygen supply;
distribute pressure evenly when occiput presents.
3. Do NOT attempt to push the cord back.
4. High flow oxygen and transport immediately while maintaining elevation of presenting
part.
Effective 1/10/23
Replaces 7/1/19
Childbirth and OB Emergencies Page 4 of 7
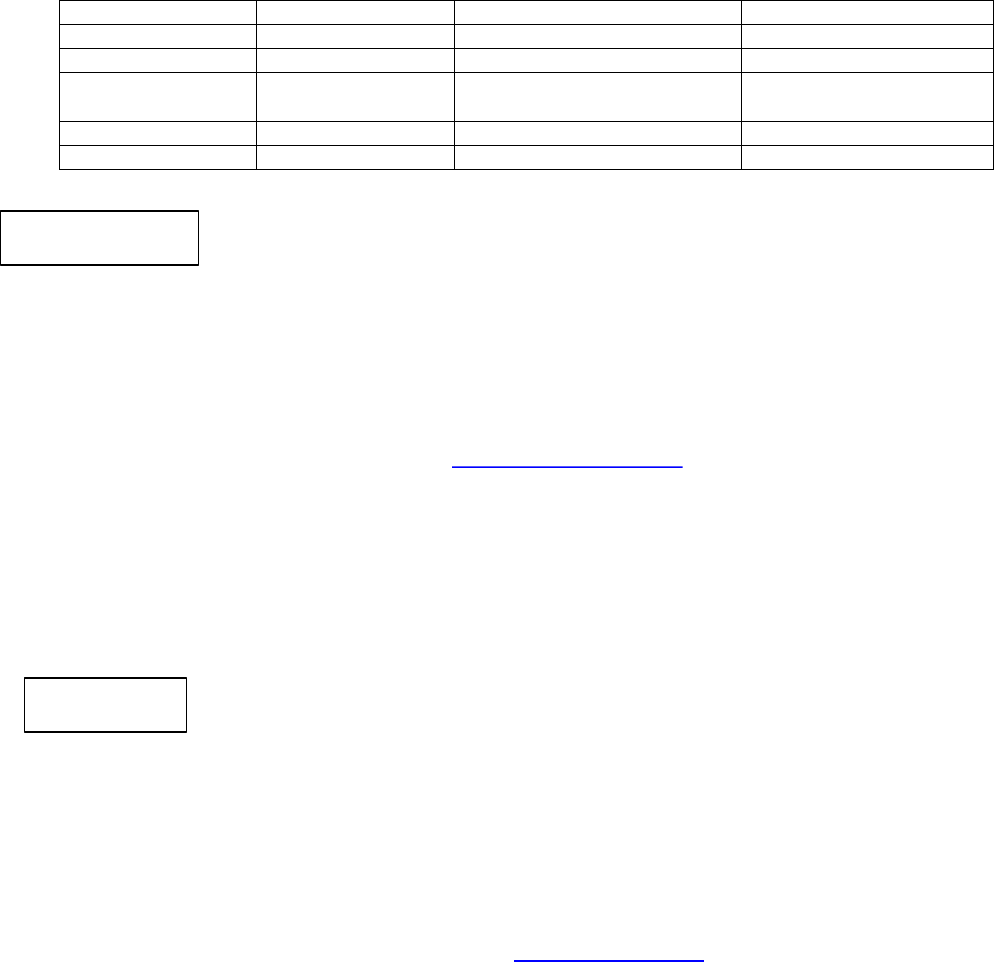
A. Approximately 10% of newborns require some assistance to begin breathing at birth. About
1% require extensive resuscitation measures. Adequate OXYGENATION is at the core of
neonatal resuscitation!
B. Those newly born infants who do not require resuscitation can generally be identified by a
rapid assessment of the following 3 characteristics:
1. Term gestation?
2. Crying or breathing?
3. Good muscle tone?
C. If the answer to all 3 questions is “yes,” the baby does not need resuscitation and should not
be separated from the mother.
1. Baby should have mouth then nose suctioned if necessary, be dried, placed skin-to-
skin with the mother, and covered with dry linen to maintain temperature
2. Observation of breathing, activity, and color should be ongoing
A. If the answer to any of the assessment questions is “no” the infant should receive one or
more of the following four categories of action in sequence:
1. Initial steps in stabilization (provide warmth, clear airway, dry, stimulate)
2. Ventilation
3. Chest compressions
4. Administration of epinephrine and/or fluid boluses
B. Approximately 60 seconds are allotted for completing the initial steps, reevaluating, and
beginning ventilation of required (see algorithm below)
C. The decision to progress beyond the initial steps is determined by simultaneous assessment
of two vital characteristics: respirations (apnea, gasping, or labored or unlabored breathing)
and heart rate (whether greater than or less than 100 or 60 beats per minute)
D. Per AHA guidelines – it is recommended that suctioning mouth then nose immediately
following birth (including suctioning with a bulb syringe) should be reserved for babies who
have obvious obstruction to spontaneous breathing or who require positive-pressure
ventilations
E. For babies born with meconium-stained amniotic fluid, endotracheal suctioning is only
indicated for depressed infants.
F. Rescue breathing is delivered at a rate of 40-60 breaths per minute. Compression-to-
ventilation ratio is 3:1, with 90 compressions and 30 ventilations delivered in one minute (120
events per minute). If cardiac arrest is suspected to be of primary cardiac etiology,
compression-to-ventilation ratio of 15:2 may be considered, but most cardiac arrests in
neonates are respiratory in etiology. Oxygenation is everything in NRP.
NEWBORN RESUSCITATION (NRP)
GENERAL CONSIDERATIONS
Effective 1/10/23
Replaces 7/1/19
Childbirth and OB Emergencies Page 5 of 7
J. APGAR scores are done at 1 and 5 minutes after delivery. Scoring should not delay any
interventions.
0 1 2
Appearance Blue / Pale Pink body, blue extremities Completely pink
Pulse Absent < 100 >100
Grimace (response
to stimulation)
No response Grimace Cough / sneeze
Muscle tone Limp Some flexion Active Motion
Respiratory effort Absent Slow, irregular Good, crying
A. You can us
e the baby’s own umbilical vein within the still attached umbilical cord to gain IV
access. Don’t forget to remove the proximal clamp
B. Start IV normal saline. If infant is hypovolemic, administer 10 ml/kg IV fluid bolus over 5-
10
m
inutes
C. Check blood sugar level, is < 40 mg/dL
administer 2 ml/kg of D10 IV
• 1 ml of D50 diluted with 4 ml of NS will yield 5 ml D10
• 2 ml of D50 diluted with 8 ml of NS will yield 10 ml D10
D. Apply monitor and check rhythm
A. In the depressed infant born with meconium-s
tained amniotic fluid, direct endotracheal
suctioning with an ET tube and meconium aspirator is indicated
B. You can use the baby
’s own umbilical vein within the still attached umbilical cord to gain IV
access. Don’t forget to remove the proximal clamp
C. If in asystole or persistent bradycardia < 60 bpm despite adequate ventilation and chest
c
ompressions administer 0.01 – 0.03 mg/kg of
epinephrine 1:10,000 IV every 5 minutes as
needed
Advanced EMT
Paramedic

NRP Resuscitation
BIRTH
30 SEC
60SEC
LABORED BREATHING OR
PERSISTENT CYANOSIS
CLEAR AIRWAY AND
MONITOR PULSE OXIMETER
POSTRESUSCITATION
CARE
TAKE VENTILATION
CORRECTIVE STEPS
INTUBATE IF NO
CHEST RISE
CONSIDER
•
HYPOVOLEMIA
PNEUMOTHORAX
HYPOGLYCEMIA
X
WARM, CLEAR AIRWAY IF
NECESSARY,DRY, STIMULATE
HR BELOW 100?
GASPING or APNEA?
VENTILATE AND MONITOR
PULSE OXIMETRY
CONSIDER INTUBATION
CHEST COMPRESSION
COORDINATE WITH
VENTILATIONS
TAKE VENTILATION
CORRECTIVE STEPS
HR BELOW 60?
HR BELOW 60?
NO
NO
NO
TERM GESTATION?
BREATHING or CRYING?
GOOD TONE?
NO
NO
NO
YES
YES
YES
YES
IV EPINEPHRINE
YES, STAY WITH
MOTHER
YES
HR BELOW 100?
HR BELOW 60?
YES
►
►
►
◄
◄
▼
▼
▼
▼
▼
YES
▼
T
H
H
▼
▼
▼
P
E
D
I
A
T
R
I
C
S
CPR RATE
3:1
90 COMPRESSIONS
30 VENTILATIONS
PER MIN
.
HYPOVOLEMIA
NS IVFs 10 ML/KG
OVER 5-10 MIN
HYPOGLYCEMIA
<40 MG/DL =
GIVE 2ML/KG D10 IV
IV EPI
0.01-0.03 MG/KG
IV PUSH q3-5 MIN
PLEASE NOTE:
This algorithm is not
Provider specific.
Expectation is that you
are to perform skills
based upon your scope
of practice.
ROUTINE CARE:
• PROVIDE WARMTH
• CLEAR AIRWAY IF NEEDED
• DRY
• ONGOING EVALUATION

Effective 1/10/23
Replaces 7/1/19
Childbirth and OB Emergencies Page 7 of 7
A. Miscarriage – premature termination of a pregnancy.
1. Assess for shock and treat per Shock Protocol
2. Give psychological support to patient and/or family.
3. Be sure to take all expelled tissue to the hospital
B. Ectopic Pregnancy – growth and development of a fertilized egg occurs outside of t
he
ut
erus; may cause massive internal hemorrhage if it ruptures
1. Patient may experience severe abdominal pain.
2. May have intra-abdominal and/or vaginal bleeding and discharge.
3. Assess for shock and treat per Shock Protocol
4. Patient may not know that she is pregnant.
5. Transport supine with knees flexed.
6. Take any expelled tissue to the hospital.
C. Cardiac Arrest
1. Precipitating events for cardiac arrest include: pulmonary embolism, trauma,
hemorrhage, and congenital or acquired cardiac disease.
2. Standard cardiac resuscitation protocols should be followed.
3. When the mother is supine, the fetus may compress the iliac vessels, inferior v
ena
c
ava and the abdominal aorta. To minimize the effects of the fetus’ pressure
on
venous return, place a wedge (pillow) under the right abdominal flank or hip, or apply
continuous manual displacement of the uterus to the left.
D. Third Trimester Bleeding
1. Abruptio placentae – premature separation of placenta from uterine wall.
Characterized by tearing abdominal pain and vaginal bleeding (may be dark). Uterus
is tender to palpation
2. Placenta previa – placenta partially or completely covers cervical os (opening);
characterized by painless vaginal bleeding (may be bright red)
3. Never perform a digital vaginal or cervical exam.
E. Pre-eclampsia
1. Hypertensive disorder that can occur during pregnancy. Can cause headaches,
vision problems, abdominal pain, nausea, vomiting, and sudden swelling of t
he
hands
, feet or face. There is no pre-hospital treatment for pre-eclampsia other t
han
t
o transport in a quiet, calm manner.
Note that mothers can develop pre-eclampsia up to 1-2 months AFTER delivery
Mild pre-eclampsia: BP > 140/90 mmHg
Severe pre-eclampsia: BP > 160/110 mmHg
F. Eclampsia
1. Serious condition characterized by swelling, hypertension and grand mal seizures.
Mothers can develop eclampsia up to 1-2 months AFTER delivery. Treatment is
magnesium sulfate and eventual delivery of the infant
Paramedic - Administer 4 grams Magnesium Sulfate in 100-250 mL of NS
infused wide open until seizure stops or total dose delivered.
OBSTETRICAL EMERGENCIES
•
• ASSESS AND MANAGE AIRWAY
•
M
AINTAIN O2 SATS >95%
• EVALUATE PATIENT CONDITION
o
CR
OWNING PRESENT WITH
CONTRACTIONS? – DELIVER ON SCENE
IF YES– SEE GUIDELINES
•
M
ONITOR VITAL SIGNS
•
OB
TAIN MEDICAL HISTORY
o
C
ONTRACTION DURATION AND INTERVAL
DUE DATE
o NUMBER OF PREGNANCIES
o
N
UMBER OF DELIVERIES OF LIVE
CHILDREN
o
P
RENATAL CARE
o
P
OSSIBLE COMPLICATIONS
• REASSURE PATIENT
•
T
RANSPORT ON LEFT SIDE TO DELIVERY
HOSPITAL WHEN POSSIBLE
•
o
o
IV NS 500 – 1000 ml BOLUS REPEATED AS NEEDED
CHILDBIRTH OB/GYN EMERGENCIES
NORMAL DELIVERIES
KEY
BASIC EMT
ADVANCED EMT
PARAMEDIC
MED CONTROL
Give TXA for post-partum bleeding
unresponsive to uterine massage and IV
fluid resuscitation
o
NORMAL PRESENTATION CHILDBIRTH DELIVERY GUIDELINES:
• GATHER EQUIPMENT – OB KIT, OXYGEN, BVM, TOWELS, BLANKETS, LARGE
DRESSINGS, COT AND PPE.
• PLACE PATIENT ON COT OR FLOOR ON HER BACK WITH KN
EES AND HIPS FLEXED.
• IF TIME PERMITS, DRAPE MOTHER W
ITH TOWELS IN OB KIT.
• DON PPE.
• AS H
EAD CROWNS, GENTLE PRESSURE WITH A FLAT HAND ON THE BABY’S HEAD
SHOULD BE APPLIED TO PREVENT AN EXPLOSIVE DELIVERY.
• SUPPORT HEAD AS IT D
ELIVERS.
• SLIDE FINGERS ALONG NECK T
O CHECK FOR THE UMBILICAL CORD.
O IF CORD PRESENT, TRY TO SLIP OVER BABY’S HEAD.
O IF UNABLE AND CORD IS WRAPPED TOO TIGHTLY FOR DELIVERY TO PROCEED,
CLAMP CORD IN 2 PLACES AND CUT BETWEEN.
• PUT HANDS ON EITHER SIDE OF INFANT’S HEAD WITH T
HUMBS TOWARDS THE
FACE.
• GENTLY GUIDE HEAD DOWNWARD TO ASSIST W
ITH DELIVERY OF ANTERIOR (TOP)
SHOULDER. DO NOT PULL! DOING SO CAN CAUSE DAMAGE TO SPINAL NERVES.
• IF SHOULDER DOES NOT DELIVER, SEE D
ELIVERY COMPLICATIONS GUIDELINES –
SHOULDER DYSTOCIA.
• GENTLY GUIDE HEAD UPWARD T
O ALLOW DELIVERY OF POSTERIOR (BOTTOM)
SHOULDER
• AFTER T
HE SHOULDERS ARE DELIVERED THE REST OF THE BODY USUALLY
FOLLOWS QUICKLY, SO BE SURE TO SUPPORT THE BODY AS IT EMERGES. INFANT
WILL BE SLIPPERY. DO NOT PUT FINGERS IN ARMPITS TO PULL THE BODY OUT.
RECORD TIME OF BABY’S BIRTH.
• SUCTION BABY”S M
OUTH THEN NOSE IF NECESSARY TO CLEAR BEFORE
STIMULATING THE BABY TO BREATHE
• KEEP BABY AT LEVEL OF VAGINA TO P
REVENT OVER OR UNDER TRANSFUSION OF
BLOOD FROM THE CORD.
• CLAMP CO
RD IN TWO PLACES ABOUT 6-8 INCHES FROM THE ABDOMEN AND CUT
• IMMEDIATELY START DRYING T
HE BABY WITH TOWELS.
• ASSESS MOTHER AND BABY FOR C
OMPLICATIONS.
• OBTAIN APGAR SCORES AT ONE AND FIVE MINUTES AFTER D
ELIVERY.
• THE PL
ACENTA MAY DELIVER ANY TIME IN THE NEXT 20-30 MINUTES. YOU DO NOT
HAVE TO WAIT FOR DELIVERY
• AFTER DELIVERY, TRANSPORT MOTHER ON COT AND BABY SKIN T
O SKIN WITH
MOM. MAKE CERTAIN BABY AND MOM ARE COVERED WITH DRY LINEN.
• KEEP MOTHER AND BABY W
ARM.
•
TRANSPORT IN POSTIION OF COMFORT
•
KEY
BASIC EMT
ADVANCED EMT
PARAMEDIC
MED CONTROL
Give TXA for post-partum bleeding
unresponsive to uterine massage and IV fluid
resuscitation
CHILDBIRTH OB/GYN EMERGENCIES
DELIVERY COMPLICATIONS
IV NS RUN TO MAINTAIN PERFUSION
• Assess and manage airway
• M
aintain O2 SATS > 95%
• Evaluate Patient condition
• Baby is breech follow guidelines
• Shoulder Dystocia-
Have mother flex hips and bring knees to chest, apply
pressure to abdomen just above the symphysis pubis
• Prolapsed Cord-
Have mother elevate hips or place in knee to chest
position, do not push on cord, use two fingers t
o
relieve cord pressure by elevating presenting part away
from cord, Administer high flow OXYGEN.
• Excessive Bleeding-
Follow shock protocol in addition to normal delivery
guidelines. Transport mother on left side if delivery not
imminent. If baby has been delivered, massage uterus
and put baby to mothers breast.
• Monitor Vital Signs
• Obtain Medical History
• Reassure Patient
• Transport to delivery hospital when possible
Breech Infant Delivery Guidelines:
• GATHER EQUIPMENT – OB KIT, OXYGEN, BVM, TOWELS, BLANKETS, LARGE
DRESSINGS, COT AND PPE.
• PLACE PATIENT ON COT OR FLOOR ON HER BACK WITH KNEES AND HIPS FLEXED.
• IF TIME PERMITS, DRAPE MOTHER WITH TOWELS IN OB KIT.
• DON STERILE GLOVES, GOWN AND FACE SHIELD.
• ALLOW BABY TO DELIVER WITH CONTRACTIONS WHILE SUPPORTING THE BODY.
THE POSTERIOR OR BOTTOM BUTTOCK AND HIP USUALLY DELIVER FIRST, THEN
THE ANTERIOR HIP.
• AFTER LEG DELIVERY, HOLD ONTO PELVIS WITH BOTH HANDS TO SUPPORT THE
BODY WHICH WILL NATURALLY TURN TO DELIVER THE SHOULDERS.
• IF THE SHOULDERS DO NOT DELIVER EASILY, APPLY GENTLE TRACTION OF THE
BODY UNTIL THE AXILLA BECOME VISIBLE. THEN GUIDE THE INFANT’S BODY
UPWARD TO DELIVER THE POSTERIOR (BOTTOM) SHOULDER. GUIDE THE INFANT
DOWNWARD TO DELIVER THE ANTERIOR (TOP) SHOULDER.
• AS THE HEAD PASSES THE PUBIS, USUALLY FACE DOWN, PUT ONE HAND ON THE
FACE AND THE OTHER ON THE BACK OF THE NECK. APPLY GENTLE UPWARD
TRACTION UNTIL THE MOUTH APPEARS.
• IF THE BABY’S BODY HAS DELIVERED AND THE HEAD APPEARS TO BE CAUGHT IN
VAGINA, THE EMT MUST SUPPORT THE BABY’S BODY AND INSERT TWO FINGERS
INTO THE VAGINAL OPENING ALONG THE BABY’S NECK UNTIL THE CHIN IS
LOCATED. AT THIS POINT, THE TWO FINGERS SHOULD BE PLACED BETWEEN THE
CHIN AND THE VAGINAL WALL AND ADVANCED PAST THE MOUTH AND NOSE.
• AFTER ACHIEVING THIS POSITION, A PASSAGE FOR AIR MUST BE CREATED BY
PUSHING THE VAGINAL WALL AWAY FROM THE BABY’S FACE. THE AIR PASSAGE
MUST BE MAINTAINED UNTIL THE BABY IS COMPLETELY DELIVERED.
• AFTER DELIVERY, FOLLOW ROUTINE NEONATAL ASSESSMENT.
OB EMERGENCIES
•
ORY
o
o TRAUMA
N
• iV Normal Saline to maintain Perfusion
• Monitor ECG
• If ECLAMPSIA Present:
Administer MAGNESIUM SULFATE 4 GRAMS in
100ml of normal saline infused wide open until
seizure stops or total dose is given
250 Normal Saline may be used
KEY
BASIC EMT
ADVANCED EMT
PARAMEDIC
MED CONTROL
• Assess and manage airway
• Maintain O2 SATS >95%
• Evaluate patient condition
MISCARRIAGE- Assess and treat for shock (see shock
Protocol ) take expelled tissue if available
ECTOPIC PREGNANCY- Assess and treat for shock, take
expelled tissue if available transport supine, knees flexed
THIRD TRIMESTER BLEEDING- Assess and treat for shock,
Transport mother on left side
CARDIAC ARREST- (See Cardiac Arrest Protocol) Transport on
left side
PRE-ECLAMPSIA- Transport in calm quiet manner
• Monitor Vital Signs-Obtain Medical History
Reassure Patient- Transport

